ASOURCE®TIMES
昭和大学 医学部 内科学講座
臨床感染症学部門 客員教授
二木芳人
1976年川崎医科大学卒業。2006年に倉敷第一病院呼吸器センターの副センター長、同年11月から昭和大学医学部臨床感染症学講座の教授等を務め、2020年4月より現職。日本感染症学会、日本呼吸器学会、日本化学療法学会など様々な学会の要職を歴任。
COVID-19の終息が見えてこない。医療現場では、いつ感染するか分からないと身構えながらの診療が続いている。昭和大学医学部客員教授の二木芳人氏は「すべての患者が感染者だと想定し、一人ひとりの医療者が感染防止策を徹底することが医療を継続する唯一の手段」と訴える。
※本取材は2020年4月14日に行われました
COVID-19の拡大が止まりません。2020年4月末時点で、全国の感染者は1万3000人、死亡者は350人を超えており、なお増え続けています。感染終息はすべての国民の願いですが、専門家でも予測のつかない状況で、ただ一つ言えるのは、新型コロナウイルスとの闘いは長期にわたるということです。
1月16日に国内で最初の感染者の報告があって以来、2月の下旬辺りまでが流行の第1波で、3月初旬から現在までが第2波ととらえられています(図)。このあと第3波、第4波……と繰り返しながら収束していくと考えています。ただし、年内の完全な終息は難しいでしょう。新型コロナウイルスは、これまでとは次元の違う手強いウイルスだと感じています。今シーズン(来春まで)、国内では20万〜30万人が感染し、死亡者も数千人レベルに達するというのが、私が描く最悪のシナリオです。
ただし、新型コロナウイルスは、気温が高く湿度が高い環境では感染力が弱くなると考えられており、8月ごろには一旦、小康状態になるとの予測もあります。ただし、涼しくなれば再び感染者が増え始めていく可能性が高いでしょう。そして来年の春にかけて、再びいくつかのピークを繰り返しながら、徐々に収束に向かっていくことが期待されています。
現在、わが国で秋〜春にかけて流行する季節性のかぜ症候群の原因となるウイルスには、インフルエンザウイルスのほか、ライノウイルス、コロナウイルス、RSウイルス、パラインフルエンザウイルス、アデノウイルスなどがあります。コロナウイルスに限っていえば、これまでに蔓延したのは4種類でしたが、新型コロナウイルスは5番目の“土着“するコロナウイルスになる可能性もあります。わが国で2009年5月に発生したH1N1亜型ウイルスによる流行は翌年3月に収束しましたが、その後ほぼ毎年、流行を繰り返しています。同様にCOVID-19も毎年流行するかもしれません。そうなると有効なワクチンが造られ、多くの人々にそれが行き渡ることがこのウイルスのパンデミックの終息には必要となるでしょう。
図1 日本国内の感染者数(3月〜) ※クルーズ船(横浜港)を除く ただし帰宅後の感染確認は含む
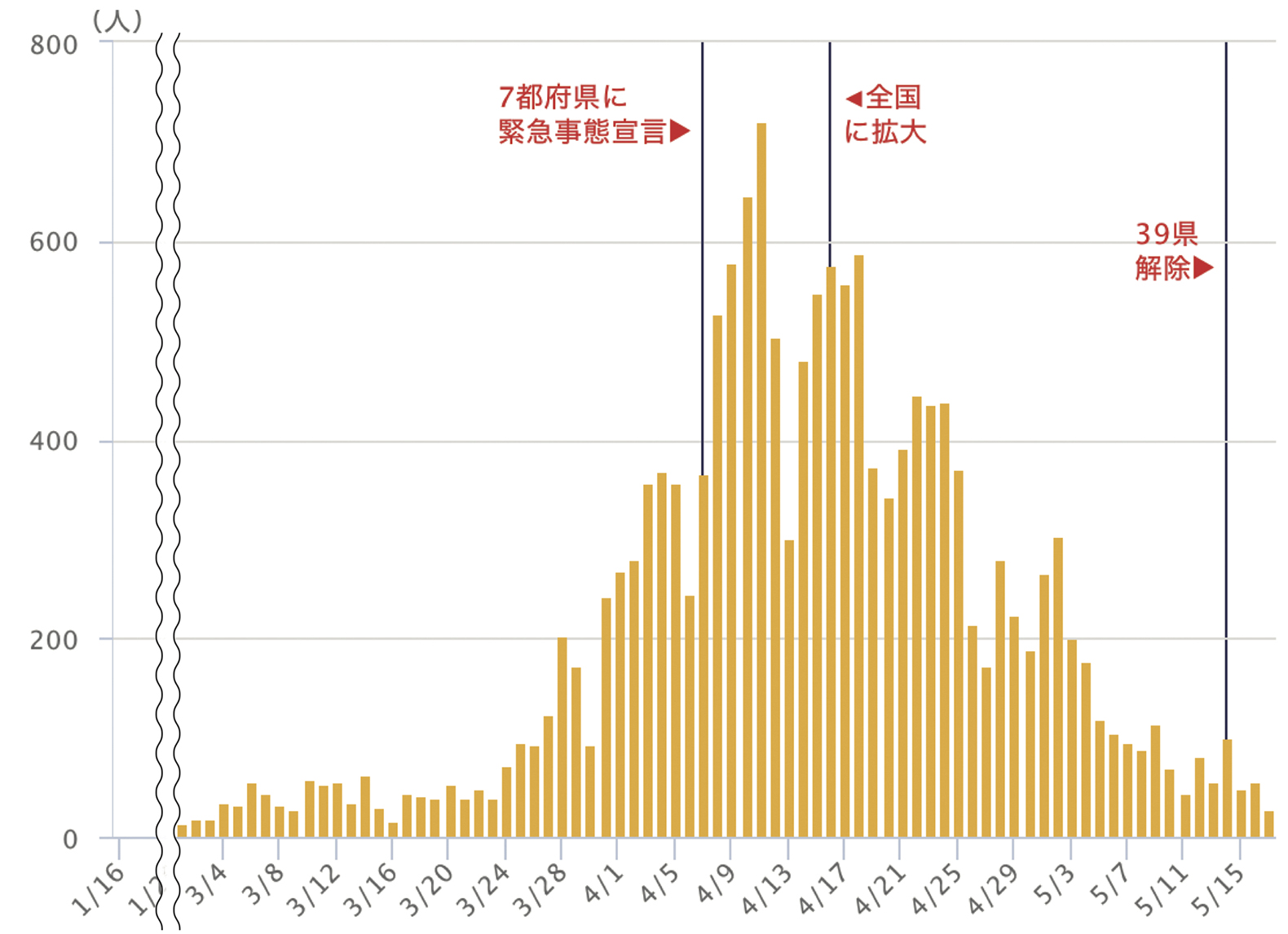
出典:NHK 新型コロナウイルス特設サイト
https://www3.nhk.or.jp/news/special/coronavirus/#infection-status
新型コロナウイルスが手強いのは、これまでのウイルスとの相違点がいくつかあるからです。まず、症状ですが、初期には鼻水や咳、発熱、軽い喉の痛み、筋肉痛、倦怠感などのかぜ症状のほか、嗅覚・味覚障害を訴える人もいます。頭痛、痰や血痰、下痢などの症状も認められます。進行すると上気道炎や気管支炎、肺炎を発症し、呼吸困難に陥ることがあります。また、最近分かったことですが、突然の重症化にはサイトカインストーム(免疫暴走)が関与している場合があるらしく、急にショックから多臓器不全を発症し、不幸な転機をとるケースが少なからずみられるようです。さらに厄介なのは、感染してもこれらの症状が出ない無症候の人や症状があまりない軽症者が多いこと、しかも無症候者、軽症者も人に感染させるため、そこから感染が広がりやすいことです。
感染経路もさまざまです。くしゃみや咳による飛沫感染のほか、感染者の手が触れたり飛沫が付いたりしたドアノブ、スイッチ、電車やバスのつり革、手すりなどに触れて感染する接触感染があります。さらに会話や呼吸で排出される1μm程度のマイクロミストやエアロゾルが空間を漂い続け、それを吸うことで感染するという指摘もあります。無症状の人が普通に生活する中で、ウイルスを無自覚に排出している恐れがあるのです。
現在の検査体制では、無症状の人はもちろん、軽症者も検査対象に含まれていません。感染しているかどうかの診断が行われないので、例えば腹痛で医療機関を受診した人が感染しているかどうかは分からず、医療機関内での感染は防ぎようがありません。事実、全国各地で病院内クラスターが発生し、高齢者施設での施設内感染も相次いでいます。そして、病院内クラスターが発生した医療機関は外来診療や新たな入院患者の受け入れを休止しています。こうした医療の機能不全が実際に起きているのです。
このような事態を防ぐためには、まず患者はすべて感染源、つまり新型コロナウイルスに感染していることを前提に、診療に当たる必要があります。サージカルマスクなどのPPE(個人用防護具:Personal Protective Equipment)を着用し、1人の患者の診察を終えたら必ず手洗いまたはアルコールでの手指消毒を行うことを徹底します。
COVID-19が疑われる症状があれば、直ちに地域の感染症指定医療機関に紹介します。ただし、最初から発熱の症状を訴える人は約4割といわれているので、典型的なかぜ症状でなくとも、問診で海外渡航歴やCOVID-19患者との接触が疑われる場合にも指定医療機関へ紹介します。
怪我などで外来を受診したり、救急外来に搬送されたりした患者にも、感染者として対処することが求められます。手袋、マスク、キャップ、エプロン・ガウン、フェイスシールド・ゴーグルなどのPPEを適切に使用し、処置中に患者が発熱や咳、息苦しさなどを訴えた場合には、X線やCT撮影で肺炎の有無を確認する必要もあります。
医療者の安全を守ることが、医療継続の基盤であり、それが患者の安心・安全、そして救命につながります。現在、マスクや手袋、ガウンなどのPPEが医療現場では不足しており、すべての医療機関にPPEを含む医療機器・材料が潤沢に供給されることが望まれます。
今回のような有事を想定した平時からの備えとしては、基本的なPPEを膨大に備蓄するべきです。これは国が備蓄するべきだと考えており、効くかどうかの保証がないワクチンを備蓄するよりも、突然流行する呼吸器系のウイルスに備えて、特にマスク、ゴーグル、ガウンなどの呼吸器疾患に適応したPPEを備蓄したほうが良いでしょう。
喫緊の課題としてはPCR検査の体制拡充です。クラスターの流れを人力で追跡する対策で、感染拡大を押さえ込める段階ではなくなりました。フェーズは変わり、より積極的にPCR検査を実施して水面下にいる感染者を拾い上げることが求められています。
PCR検査の結果と診察で、患者を症状の程度別に振り分け、それぞれ別の対応をする必要があります。流行の初期の頃はこの振り分けが適切にできておらず、人数の多い軽症者が病床を占めたために、重症者のベッドが不足するという事態が起きました。地方自治体によっては、軽症者を「自宅待機」とするようになりましたが、これこそが医療崩壊の兆しです。家族内感染の危険が高く、一人暮らしの人でも、生活必需品の調達のために外出して感染者を増やす危険もあります。加えて、一人暮らしの人では急変に素早く対応できず、不幸な転機をとるケースも報告されています。
こうした現状を踏まえ、今後は医療機関と国・地方自治体との連携を一層強化し、迅速かつ適時、的確な対策を講じることがCOVID-19の終息には不可欠だと考えています。