Japan's disaster medicine system is in place every time a natural disaster is experienced, and the number of medical institutions that formulate business continuity plans (BCPs) is gradually increasing. In the future, it will be necessary to develop a “support” plan to continue medical care by successfully accepting supporters and relief supplies after a disaster.

The full-scale efforts for disaster medicine began in Japan after the Great Hanshin-Awaji Earthquake that occurred in January 1995. More than 6,400 people were killed in the disaster. However, it is estimated that hundreds of people could have saved their lives if the medical institution had a disaster response system in place.
The main problems related to medical institutions at the time of the Great Hanshin-Awaji Earthquake, which were confirmed after the disaster, were the disruption of lifelines, damage to the buildings and equipment of medical institutions, concentration of victims, and lack of information sharing with surrounding medical institutions. There was insufficient medical care in the acute phase, undeveloped methods for transporting patients to the outside of the disaster area, and there was no way to directly or indirectly support the disaster area from outside the disaster area.
Based on these lessons, a disaster base hospital was established after 1996 after the Great Hanshin-Awaji Earthquake, and a disaster dispatch medical team (DMAT) was born. In the disaster area, a system has been put in place such as collecting patients at a medical relief center, triage them, and then transporting them to a disaster base hospital for treatment, and in the case of a major disaster, transporting them to a wide area outside the disaster area by helicopter.
After that, in the Great East Japan Earthquake that occurred in March 2011, the system of this medical rescue station and disaster base hospital was tried. At that time, a medical relief center was set up in the disaster area, but it is said that many of the affected patients gathered at medical institutions rather than medical relief centers without IV stands and medicine racks. In fact, in the acute phase after the disaster, it was difficult to collect medical personnel, medical equipment, and medicines at the medical relief center, and it seems that it was easier for medical institutions that had no damage and had medical equipment. On the other hand, due to the damage from the tsunami, some disaster base hospitals were unable to carry out medical activities.
At that time, hospitals other than the disaster base hospitals were dealing with many patients, including originally inpatients and new patients. However, it became clear that the medical plan designed before the Great East Japan Earthquake did not include medical institutions other than the disaster base hospital, so that relief supplies from the government did not arrive.
It is necessary to have a disaster medical plan based on the phase in which such experience gradually shifts from independent activities in the turbulent period immediately after the disaster to orderly organizational activities, and medical resources are drastically reduced in the acute period when medical demand increases sharply. I learned that it is necessary to have a decision-making department that can respond to unexpected situations and to respond with all-out efforts in order to do so, which led to the movement to formulate a business continuity plan (BCP) for medical institutions after the Great East Japan Earthquake. go.
BCP became a growing concern for companies in the United States and the United Kingdom in the 1970s as a way to continue their business in an emergency, and after the terrorist attacks in the United States in September 2001, many worldwide. Companies have come to think seriously about the importance of business continuity. In Japan, this idea did not easily permeate companies, and only 7.8% of companies formulated BCP before the Great East Japan Earthquake. However, after the earthquake, it is said that the number of companies that formulate BCPs and improve or review the formulated BCPs has tripled.
On the other hand, regarding the BCP of medical institutions, for example, the Bureau of Social Welfare of Tokyo published the "Business Continuity Plan (BCP) Guidelines for Medical Institutions in the Event of a Large-Scale Earthquake Disaster" in 2012, and illustrated the concept of BCP for medical institutions. The government has started to support the formulation of BCP (Fig. 1). However, following these movements is only a part, and in the "Fact-finding Survey on Business Continuity in Specific Fields" released by the Cabinet Office in August 2013, 7.1% of medical institutions' BCPs were "already formulated" and "under formulation". Was 10.3%, which was lower than other industries.
Under these circumstances, the Kumamoto earthquake, which observes seismic intensity 7 twice, occurred in April 2016. Since both the pre-earthquake and the main earthquake occurred at night, medical institutions were forced to call staff urgently, and the lifeline and the building of the medical institution were damaged, making it difficult to provide continuous medical care and hospitalization instead of accepting patients. It is fresh in my memory that there were many cases of "hospital evacuation" in which patients were transferred to other medical institutions.
For this reason, in 2017, the Ministry of Health, Labor and Welfare added the formulation of BCP as a requirement for designation of disaster base hospitals in the notification of "Partial revision of requirements for designation of disaster base hospitals". The contents are that the business continuity plan is being prepared so that the medical care function can be restored at an early stage after the disaster, and that training and training assuming the disaster situation will be carried out based on the prepared business continuation plan, and the area. We have established a system to carry out regular training with medical institutions such as the Second Emergency Medical Institution, the Regional Medical Association, and the Japanese Red Cross Society, and to provide support to regional medical institutions in the event of a disaster. It is supposed to be.
In addition, considering that many medical institutions do not have the skills and know-how necessary for BCP maintenance and lack information on the contents of BCP, we are targeting BCP planners at disaster base hospitals. We started a training project on building a BCP formulation system, grasping the current situation and assuming damage, organizing priority work for business continuity, and documenting action plans.
The Kumamoto earthquake caused damage to buildings and medical equipment at about 1,300 of the 2,500 medical institutions in the prefecture. There was a medical institution that had to evacuate to the hospital even though it had prepared a disaster countermeasure manual and trained to accept a large number of injured and sick people. This is because the disaster countermeasure manuals of each medical institution assumed that the buildings and equipment of their own hospital would not be damaged. Therefore, what has come to be emphasized is BCP based on the perspective of which work should be carried out by when, by organizing the work that should be prioritized in advance, assuming that medical resources will be limited immediately after a disaster. ..
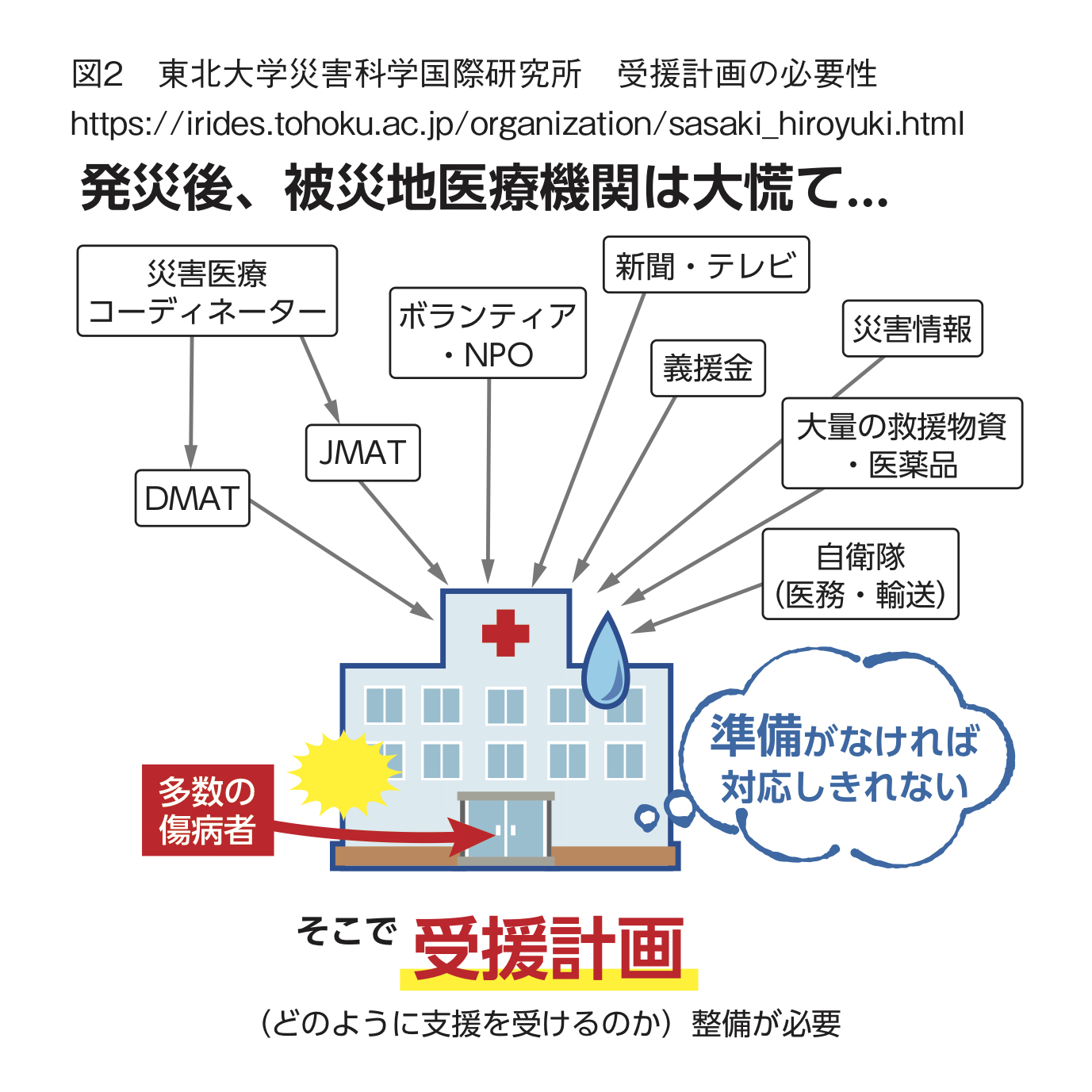
Also, at the time of the Kumamoto earthquake, few medical institutions expected to prepare for accepting supporters such as DMAT. Hiroyuki Sasaki, an associate professor at the International Research Institute of Disaster Science, Tohoku University, said, "In order for medical institutions to continue their business in the event of a disaster, it is necessary to have the idea of" support "to successfully accept the support of people and things that are in short supply." Emphasize (Fig. 2). When a disaster occurs, support teams are quickly dispatched from all over the country and relief supplies are sent. However, the affected organizations on the receiving side, including medical institutions, are busy with the immediate response and cannot fully utilize the wave of support.
To receive support, it is first necessary to secure a meeting space for the support team to be dispatched and a warehouse space for storing and organizing relief supplies. When providing usable medical equipment / materials and pharmaceuticals, we will timely grasp the medical resources that the supporters lack, consider what kind of medical resources will be needed in the future, organize these and provide information. You must make a call and receive appropriate support.
Mr. Sasaki said, "Three elements are essential for BCP of medical institutions. It is to clarify" business priority "," secure alternative means "to continue essential functions even if a disaster occurs, and disaster. It's "management of medical resources" to maintain its function at times. " In recent years, natural disasters such as typhoons and floods have paralyzed the medical functions of the region almost every year. In order for a medical institution to function as a social infrastructure in the event of a disaster, the idea of support should be firmly established in the medical institution itself, and a BCP that clarifies the role to be played should be formulated to improve its effectiveness while improving the content on a daily basis. It is important to keep going.
 Necessity of Support Plan, International Research Institute of Disaster Science, Tohoku University
Necessity of Support Plan, International Research Institute of Disaster Science, Tohoku University