ASOURCE®TIMES
院内感染が発生した場合、その封じ込めのための多大な労力とコストが必要となるだけでなく、病院の評判にも関わる危機的な状況に陥る。すなわち、健全な病院運営を遂行する上で欠かせないのが院内感染対策といえる。具体的には、手指衛生の徹底、針刺し損傷の防止、器具の適切な洗浄・消毒・滅菌などが重要とされ、院内感染に対する病院スタッフの意識の向上が求められる。

これまで主に院内感染の原因菌としてクローズアップされていた耐性菌が市中においても広がりをみせている。メチシリン耐性黄色ブドウ球菌(MRSA)のように有効な抗菌薬がある場合もあるが、多剤耐性緑膿菌、多剤耐性アシネトバクター、NDM-1産生菌、KPC産生菌といった高度な耐性を示す菌に対しては使用可能な抗菌薬も限られる。九州のある大学病院では、昨年4月から今年4月にかけて、同院に入院していた患者5人から多剤耐性アシネトバクターが検出され、うち3人が死亡している。
院内で耐性菌の感染源となるのは、主に排菌している患者であり、患者に耐性菌が伝播する経路としては、①患者→患者、②患者→院内環境→患者、③患者→医療器具→患者、④患者→医療スタッフ→患者の4つのルートが考えられる。院内のアウトブレイクを防ぐためには、これらの伝播経路の全てを遮断する必要があるが、中でも接触の頻度から考えると、医療スタッフの手指衛生がもっとも効果的と考えられている。
医療現場では、「忙しくて手指衛生が徹底できない」という声も聞かれるが、感染対策の意識を持って日常の業務を行ってもらうよう、定期的な教育や啓蒙活動による意識の向上が望まれる。従来はポンプ式のものが多かったが、最近は自動で手指消毒剤が吐出されるノータッチ式ディスペンサーが普及している模様だ。
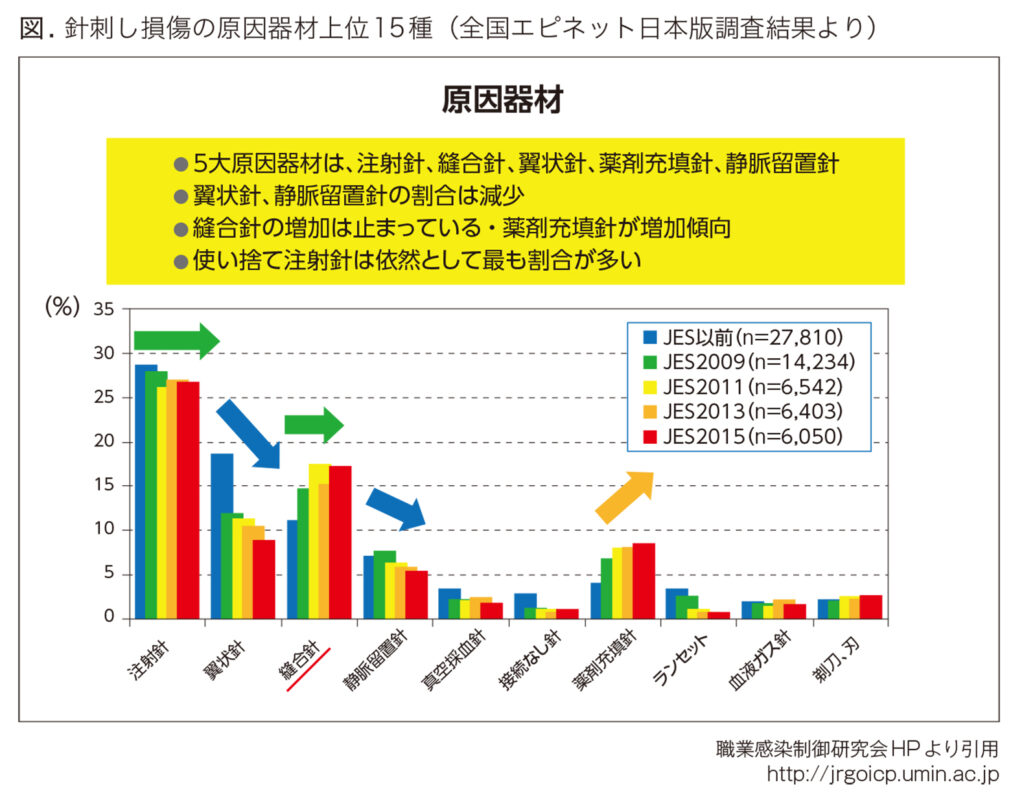
医療従事者の感染防止対策として針刺し損傷を防ぐことも重要な課題である。針刺し損傷は、年間5万件報告され、推計で約20万件発生している。血液媒介病原体への新規感染の約3分の1が医療関連感染とされる。職業感染制御研究会によると、受傷者は、看護師が過半数を占め圧倒的に多いが、近年看護師の割合が減少し、医師の割合が増加傾向にある。針刺し損傷の発生場所は、病室、手術部、病室外で全体の7割を占める。発生時期は、➀患者へ使用後に破棄容器に収容するまで②患者に使用中③リキャップ時の3要因で約60%を占める。針刺し損傷の原因器材上位15種のうち注射針による針刺しが最も多く報告され、採血やインスリン注射、薬剤の筋注など、多くの場面で注射針による針刺し損傷が発生していることが推測されている。翼状針の針刺しは「安全機構付き」の普及により減少しているが、薬剤充填針の増加が目立っている(図)。ある医療機関の看護師が採血時の針刺し損傷により患者血液からC型肝炎に感染したケースでは、訴訟に発展し、医療機関の安全義務が問題となった。厚生労働省の院内感染防止の通達(リキャップ禁止、破棄容器の適切配置、安全器材の活用)のさらなる実効性を上げる努力が望まれる。
ただし、安全対策製品の普及については依然課題が残されている。安全装置付きの静脈留置針が従来品より償還価格が高く設定されているため普及が進んでいる一方で、セーフティシリンジ製品については、価格が高く、償還価格に利点がないことがネックとなり、普及が遅れている。注射針による損傷が最も多い要因である現状を踏まえると、償還価格の見直しも検討課題の1つといえる。
近年、医療施設において感染対策の重要性がクローズアップされ、使用済み器材の適正処理が感染拡大防止の基本であるという認識が広がりつつある。
大規模病院では、院内感染対策としてトレーサビリティシステムを導入する施設が増えつつある。費用はかかるが、感染防止や滅菌保証のフォローアップにつながるものとして注目されている。使用頻度や耐用年数の器材情報から金属疲労による破損リスクの低減、器材購入時期の目安の判断など、利点が多く、患者への危険回避のほか、器材を扱う医師・看護師にとって負担軽減につながるものとみられている。
眼科領域では、手術における感染リスクの低減には再生処理が難しい器材のディスポーザブル化が必要不可欠とされ、洗浄機で洗浄が困難な器材に関しては可能な限りディスポーザブルを採用しているところが多いという。光源付き器材、白内障の手術に使用するUSハンドピースやJ/Aハンドピースの先端部などがこれに当たる。
一方、多くの医療従事者のユニフォームの洗濯は病院が契約している専門のクリーニング店か白衣を提供しているリース会社が行っているが、院内で洗濯業務を行う施設もある。医療用ユニフォームは黄色ブドウ球菌をはじめ様々な病原菌によって汚染され、血液が付着する場合もある。ユニフォームの交換は、細菌学的見地から考えると、毎日が望ましいとされるが、実際には、週1回程度が多いようだ。ユニフォームの洗浄方法は施設によって異なるとされるが、酵素系洗剤などを使った適切な洗浄が求められる。感染対策の面からもガイドライン作成や診療報酬上の加算措置などが求められる。