ASOURCE®TIMES
これまで医療における位置づけや定義があいまいであったオンライン診療が、平成30年度診療報酬改定で本格的に評価されることになった。その背景には、スマートフォン(スマホ)の普及も含めた情報通信技術(ICT)の進歩がある。平成30年度からはオンライン診療が診療報酬制度において明確に位置づけられ、ガイドラインもできたため、求められる要件は従前よりも厳しくなった。新しい展開を踏まえて、オンライン診療の今後の展開を探る。

平成30年度診療報酬改定における基本的視点は、①地域包括ケアシステムの構築と医療機能の分化・強化、連携の推進、②新しいニーズにも対応でき、安心・安全で納得できる質の高い医療の実現・充実、③医療従事者の負担軽減、働き方改革の推進、④効率化・適正化を通じた制度の安定性・持続可能性の強化――の4つである。
今回は6年に一度の介護報酬改定と同時であるため、地域包括ケアシステムを構築するという観点から、介護保険制度との整合性や連携を図ることに力点が置かれたのが特徴だ。
平成30年度診療報酬改定において評価された遠隔診療あるいはオンライン診療は、前述の4つの基本的視点のうち②に位置づけられている。そこでの柱の一つである「先進的な医療技術の適切な評価と着実な導入」において、「遠隔診療の評価」が挙げられた。
その③の視点も注目される。現在、政府や厚生労働省(以下「厚労省」)が「働き方改革」を推進しており、その一環として、ICTを活用して医師の負担軽減を図ろうとしている。特に医師不足の地域では、ICTを活用した診療が有用・有効と考えられる。
平成30年度からの診療報酬体系では、遠隔診療を「医師対医師」、「医師対患者」に大別する。(表1)
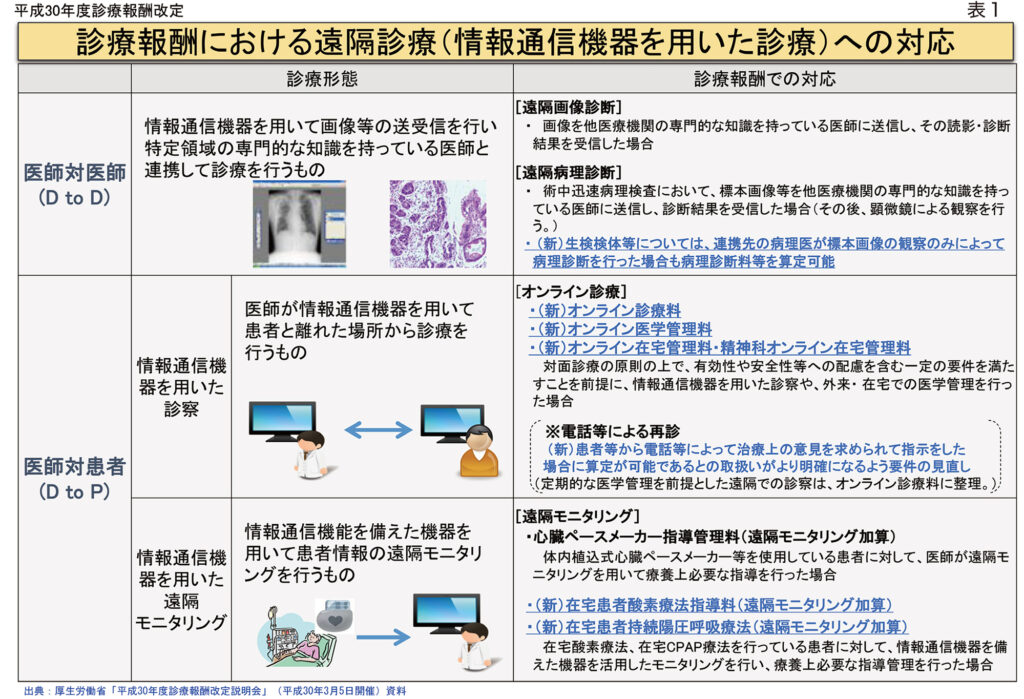
「医師対医師」(通称「D to D」)は、例えば遠隔画像診断、遠隔病理診断などである。この「D to D」については、従前から診療報酬上の算定は行われていた。ただし、遠隔で病理診断を行う場合は、病理標本を送付しなければならなかった。今回、患者から採取した標本画像(デジタル病理画像)を他医療機関の専従の医師に送信して、その結果を受信した場合もOKとなった。
「医師対患者」(通称「D to P」)は、さらに「通信機器を用いた診察」(オンライン診療)、「情報通信機器を用いた遠隔モニタリング」に分かれる。平成30年度診療報酬改定で新たな評価がなされたのは、主として「D to P」の診療形態である。特にオンライン診療に当たるものに、例えばオンライン診療料、オンライン医学管理料、オンライン在宅管理料など、新たな報酬体系が導入された。
今後、「医師対患者」での遠隔診療において中心をなすのは、オンライン診療料(70点、1月につき)、オンライン医学管理料(100点、1月につき)だ。
既存の診療報酬の体系は、基本診療料(初・再診料、入院料等)、特掲診療料(医学管理等、在宅医療、検査、画像診断ほか)に大きく分かれる。それに当てはめれば、オンライン診療料は再診料(あるいは外来診療料)の類型である。そのため、従前の「電話等による再診」の要件も見直し、整理がなされた。また、オンライン医学管理料は、特掲診療料での「医学管理等」における新たな加算に相当する。
したがって、初診は必ず対面診療とし、以後も定期的に対面診療を行うことが原則だが、オンライン診療料とオンライン医学管理料を合わせて算定することもできる。
オンライン診療料が算定可能なのは、特定疾患療養管理料、地域包括診療料、小児科療養指導料、認知症地域包括診療料、てんかん指導料、生活習慣病管理料、難病外来指導管理料、在宅時医学総合管理料、糖尿病透析予防指導管理料、精神科在宅患者支援管理料を算定していて、それらの管理料を初めて算定した月から6月以上を経過した患者である。このように、生活習慣病を中心に、小児や在宅医療など幅広い対応ができるようになっている(表2)。
オンライン医学管理料の対象となるのは、特定疾患療養管理料、小児科療養指導料、てんかん指導料、難病外来指導管理料、糖尿病透析予防指導管理料、地域包括診療料、認知症地域包括診療料、生活習慣病管理料を算定していて、初診から6月以上を経過した患者である。療養計画に基づいて対面診療とオンライン診療を組み合わせて医学管理を行い、前回受診月の翌月から今回受診月の前月までの期間が2月の場合に限り、所定の管理料に合わせて算定できる。ただし、対面診療で特定疾患療養管理料などを算定する月では、オンライン医学管理料は算定できない。
具体的にどのような通信機器を用いたネットワーク環境でオンライン診療を行うことが望ましいのか、厚労省は「情報通信機器を用いた診療に関するガイドライン作成検討会」を設置し、検討を続けている。平成30年3月9日に開催した第2回同検討会で、同省は「オンライン診療の適切な実施に関する指針(案)」を提出し、大筋で合意を得たうえで、パブリックコメントとして国民の意見を求め始めた。同月29日に開催された第3回同検討会で「オンライン診療の適切な実施に関する指針」が最終的にまとまった。
同指針が適用される具体例として、①高血圧患者の血圧コントロールの確認、②離島の患者を骨折疑いと診断し、ギプス固定など処置の説明等を実施、③医師が患者に対して問診を行い、適切な診療科への受診勧奨を実施(オンライン受診勧奨)、などが挙げられている。また、「最低限遵守する事項」「推奨される事項」「望ましい例」「不適切な例」などを示しており、実用的なガイドラインとなりそうだ。
オンライン診療における患者側の端末について、「オンライン診療の適切な実施に関する指針」では、患者個人が契約するスマートフォン等による利用が想定されるとしたうえで、それによる不正アクセスを防止するため、例えばID/パスワードの設定など、患者の端末における適切な本人確認(認証)を実施すること、としている。また、患者側では、ノートパソコンに組み込まれたカメラとマイクを使って通信したり、パソコンとスマホを組み合わせる方法も想定されるが、この場合も、同様の注意が必要だ。
また、平成29年5月30日に施行された改正個人情報保護法では、病歴や健康診断等の結果は「要配慮個人情報」として、不当な差別や偏見その他の不利益が生じないように取扱いに特に配慮を要するもの、とされた。患者が会社の昼休みにオンライン診療を希望することも想定されるが、会社の同僚がいるところでオンライン診療を実施することなどは極めて問題があるといえる。
それらの点を考慮すれば、患者側としても、自宅/在宅の落ち着いた環境でオンライン診療を受けることが望ましい。実際には、さまざまな疾患の患者がオンライン診療の対象となり、それぞれの患者にとって適切な時間帯もある。医療機関側としても、特定の時間帯にどこまでオンライン診療の予約を受けられるかが、対応のポイントとなりそうだ。
実際診療では、事前に診療時間を予約。時間がきたらスマホやパソコンを立ち上げ、診療所などの医師と回線をつなぐ。医師は患者の顔を見ながら「お変わりありませんか」などと話を切り出し診察を開始する。患者にとって通院時間や待ち時間がないのが大きなメリットだ。高齢者は足が弱っていたり、付き添いが必要な場合も少なくなく負担が軽くなる。処方箋は郵送で受け取る。支払いはクレジットカードなどで行う場合が多いという。また、オンライン診療は、訪問診療でも威力を発揮しそうだ。患者や家族が医師の顔をみて相談できれば、安心感が得られ、医師側の訪問の負担も軽減される。
一方、医療機関同士の遠隔医療としては、昭和大学では、重症部門向けの遠隔医療の仕組みの1つである遠隔集中治療患者管理プログラム(eICU)の導入を始めている。eICUにより、同病院と昭和大学江東豊洲病院の集中治療室(ICU)50床を一括して24時間遠隔管理する。eICUでは、モニター上で各患者の状態の変化が把握できるだけでなく、病院内での重症患者の位置関係がすぐにわかるので、重症部門のベットを効率的に運用できる。現場のスタッフと遠隔地の医師とで治療方針の相談ができる利点もある。ICUに入る高齢患者が増える一方で、集中治療専門医は不足しているため、先端システムによる管理で、医療の質が担保できる。米国ではeICUの導入で重症患者の死亡率が改善したり、入院日数の短縮が認められるという。また、旭川医科大学では、中国の中日友好医院(北京市)と瑞金医院(上海市)の2医院とで遠隔医療を行っており、放射線科の画像読影や眼科診療、病理診断などの支援をしている。
遠隔診療が評価されるまでにはいろいろと経緯があった。平成9年遠隔診療通知では、遠隔診療の対象について「直接の対面診療を行うことが困難である場合」として、「離島、へき地の患者」などを例示していた。それについて平成27年遠隔診療事務連絡では、あくまでも例示であると強調。また、平成29年遠隔診療通知では、テレビ電話、電子メール、ソーシャルネットワーキングサービス(SNS)等の情報通信機器を組み合わせた遠隔診療についても、直接の対面診療に代替し得る程度の有用な情報が得られる場合には、直ちに医師法第20条(無診察治療等の禁止)等に抵触するものではない、と説明した。
その事務連絡や通知により、遠隔診療が違法でない領域がある程度明確になったため、大都市を中心に、遠隔医療に積極的に取り組む医療機関が出始めた。仕事で忙しく、通院が難しい生活習慣病患者などにおいては、遠隔診療の利便性・有用性が認められるようになった。しかし、診療報酬上の位置や評価は明確でなかった。厚労省としても、そのような状況を放置できず、今回、遠隔診療を診療報酬体系に組み込み、一定の規制をかけたうえで、その普及を図ることになった。