ASOURCE®NAVI

公開日:2021.02.15
緊急事態宣言下の地域では、新型コロナウイルス感染者の急増に伴い、入院患者が受け入れられないケースが生じ、「医療崩壊」が懸念されています。日本は欧米諸国に比べて人口当たりの病床数が多く、感染者数はより少ないのに、なぜ病床はひっ迫しているのでしょうか。
経済開発協力機構(OECD)がまとめた最近のデータによると、人口1,000人当たりの病床数は日本が13.0床で、主要7カ国では、ドイツ8.0床、フランス5.9床、イタリア3.1床、米国2.9床、英国2.5床などに比べて圧倒的に多くなっています(図1)。急性期の病床に限っても日本は7.79床で加盟国の平均3.6床に比べて2.2倍以上突出しています。病院数は2016年のデータでは、日本は8,442カ所と最も多く米国の1.5倍となっています。
1位 8,442 日本
2位 5,564 アメリカ
3位 4,474 メキシコ
4位 3,788 韓国
5位 3,100 ドイツ
6位 3,065 フランス
7位 1,922 イギリス
8位 1,510 トルコ
9位 1,331 オーストラリア
10位 1,086 イタリア
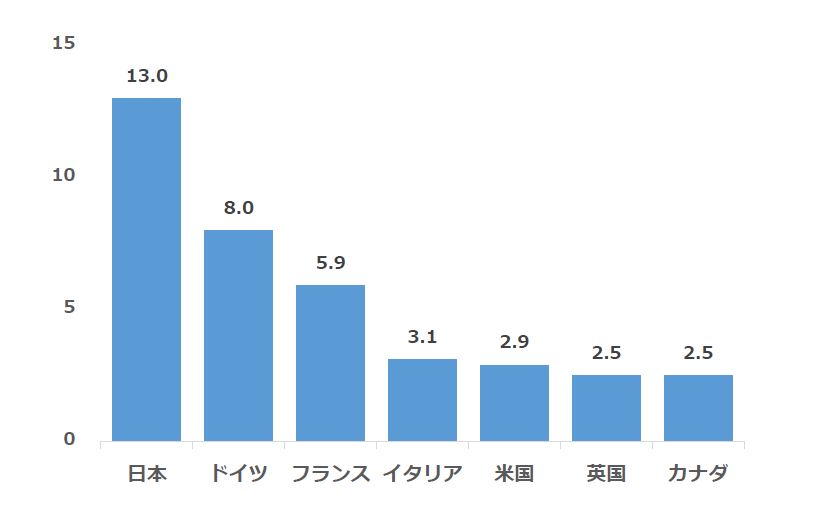
図1 人口1000人あたりの病床数 出典:OECD
しかし、日本のコロナ向け病床は約2万8,000床で、感染症への対応が可能な病床全体約73万床の4%弱にとどまるとされます。重症者向けの確保予定病床数も約3,600と横ばいの状態といわれています。厚生労働省の昨秋の調査によると、急性期病棟を持つ4,201病院の新型コロナ患者の受け入れ実績があるのは、公立病院53%、公的病院69%、民間病院14%でした(図2)。
欧州では、多くの病院が大規模な公的病院で、行政の意向を反映しやすいといわれ、コロナ禍において政府主導で短期間に集中治療室(ICU)を増やすなどの対応を可能にしてきました。また、特定の医師をかかりつけ医とする制度が定着しています。例えば、ドイツでは2004年に「家庭医制度」、フランスでは2007年に「主治医制度」を導入しました。患者は、まず自分が選択した医師を受診し、必要に応じて他の専門医などの紹介を受けます。医療従事者の不足が懸念されるなか、一次医療をかかりつけ医、二次以降の医療を専門医や病院が担うという役割分担の明確化は、医療資源の有効活用という観点からも重要です。わが国においても、欧州のように特定の医師をかかりつけ医とする制度の導入を早急に検討すべきとの指摘があります。
コロナ病床がひっ迫する背景の1つとしては、医療スタッフ数が十分とはいえないことが指摘されています。OECD データによると 、日本の医師数は、人口1,000人当たり2.5人で、データで示された35か国中28位で、ドイツ4.3人、フランス3.4人、英国3.0人、米国2.6人と比べても少なくなっています(図3)。コロナ重症患者が入るICUの専門医もドイツには約8,000人いますが、日本は2,000人近くにとどまります。
重篤な新型コロナウイルス患者の治療に使われるのが、人工心肺装置「ECMO(エクモ)」ですが、日本呼吸療法医学会の調査によれば、日本には1,400台のECMOがあり、世界でも有数の保有台数を誇っています。しかしECMOの操作が可能な臨床工学技士は1000人以下と少なく、ECMO操作は2〜3交代で24時間態勢で動かす必要があり、実際に常時実働できるのは300人程度になるとみられています。さらに「医師」「看護師」「臨床工学技士」の3人でチームを組むため、臨床工学技士以外にも多数のスタッフが必要となり、治療にあたるスタッフが不足しています。
コロナ患者への対応は、一般患者の倍の手間がかかるとされます。しかしながら、日本では、病院全体の約8割を占める民間病院の多くが200床以下の中小規模で、スタッフが限られ、感染症対策の設備も整っておりません。もともと人口1000人あたりの医療従事者数が少ないうえに、小規模病院に人員が分散してしまっていることも病床逼迫の背景の一つとなっています。
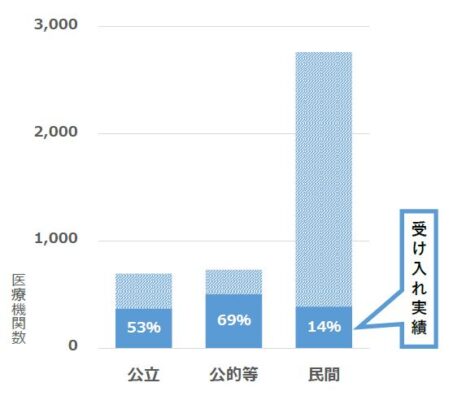
図2.急性期病院の新型コロナ 患者の受け入れ実績 厚生労働省調べ 2020年9月末時点
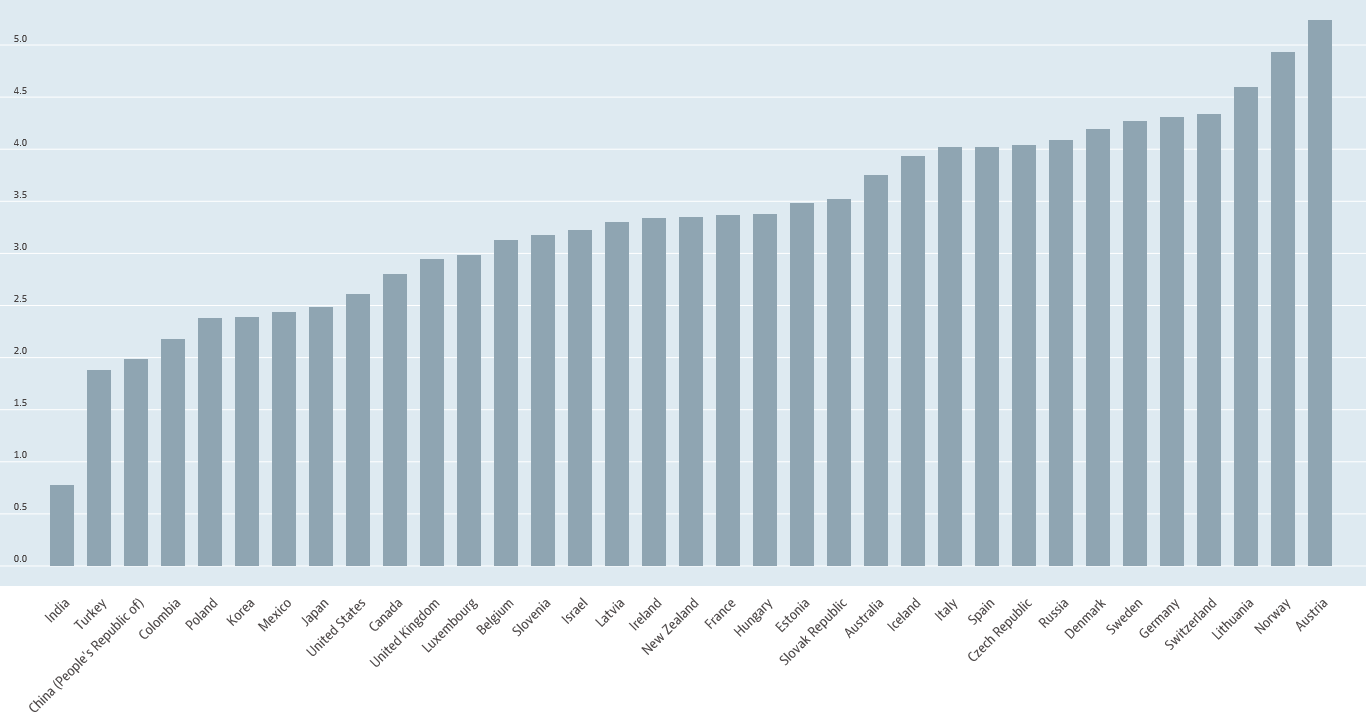
図3.人口1,000人当たりの医師数の国際比較 出典:OECD
コロナ病床ひっ迫のもう1つの背景としては、日本の医療制度の構造的な問題が存在します。民間病院は常に病床を満床に近い状態にしないと経営が成り立ちにくいということがあり、空き病床が少ないとされます。感染症の専門医が少なく、スタッフが感染対策に不慣れな点もあります。いったん院内でクラスター(感染者集団)が発生すると、病院の信用が揺らぐほか、場合によっては、病床閉鎖や入院制限を余儀なくされ、病院の経営に極めて大きな打撃となりかねません。コロナ患者を受け入れることで病院への風評被害が起きるケースも報告されています。すなわち、コロナ患者を受け入れると病院の収益が減少するリスクが大きく、赤字でも税金投入で維持される公立病院とは違うところです。
現在、コロナ病床確保の問題については⓵中小病院にコロナから回復した患者の受け入れを拡充してもらう、⓶時限的にコロナ対応病院の病床を拡大し、その通常医療機能を中小病院に代替してもらう—などが検討されています。民間病院の医療資源をうまく活用するとともに、病院間の連携や機能分担をいかに実効性のあるものにしていくかが問われています。
メディアスグループは、医療機器の販売を中心とした事業を展開しています。医療に携わる私たち(Medical+us)は、医療現場や人々の健康的な明日へ役立つ情報をお届けする情報発信源(Media)の役割も果たしていきたいと考えています。