ASOURCE®NAVI

公開日:2024.05.10
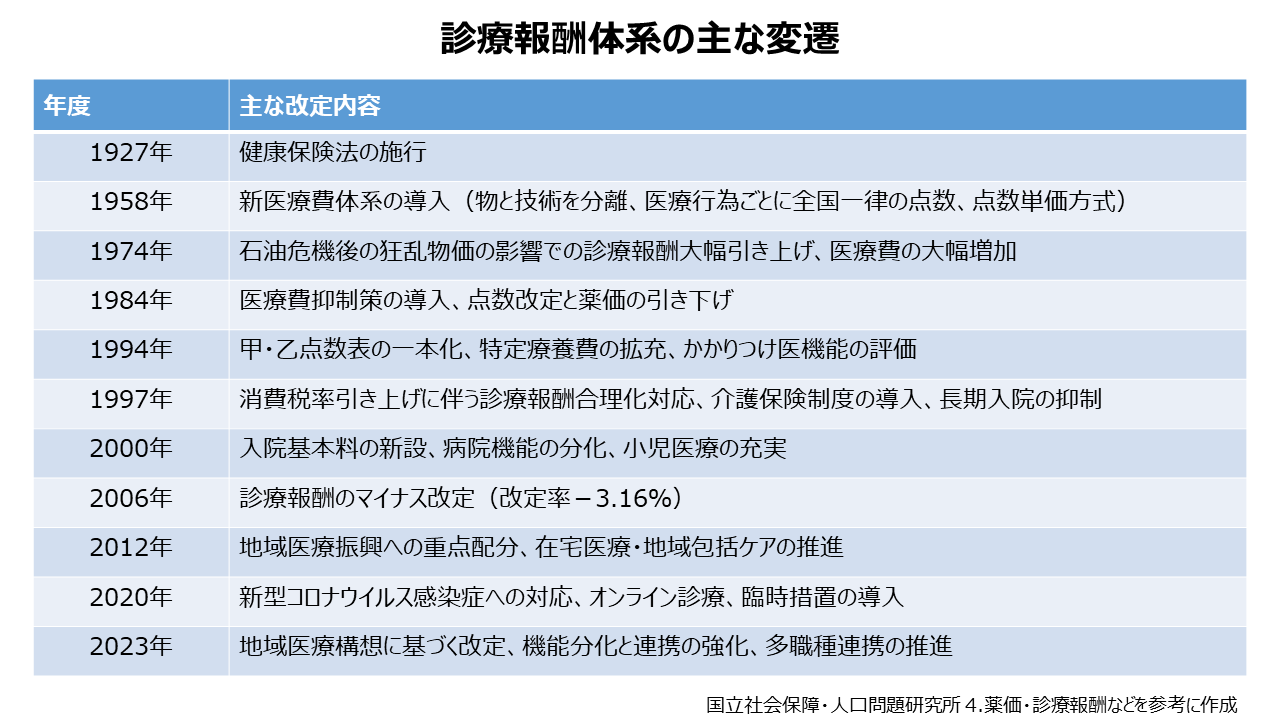
日本の診療報酬体系は、国民皆保険制度の基盤となる重要な仕組みであり、医療の質と効率を左右する役割を担っています。その歴史は1927年に健康保険法が施行されてから始まり、幾度かの変遷を経て現在に至っています。今回は、診療報酬改定の歴史をまとめます。
医療現場ではさまざまな診療行為が行われていますが、診療報酬制度は、これらの医療サービスと使用された物品に適正な対価を支払う仕組みとなっています。診療報酬は、保険医療機関および保険薬局が保険医療サービスに対する対価として、保険者から受け取る報酬です。診療報酬の内容は、技術・サービスの評価と物の価格評価(医薬品は薬価基準にて価格決定)となっています。これらの評価基準は、厚生労働省により公的医療保険の範囲内で定められています。実際の診療後は、医療機関が行った診療行為の点数を合計し、1点10円として総額を算出します。患者はその一部(1~3割)を自己負担しますが、残りの金額は審査支払機関を経て保険者から医療機関に支払われます。診療報酬の点数は、医療の進歩や経済状況、実際の市場価格などを踏まえて、通常2年に一度見直しが行われています。これらは、国の医療政策に医療機関を誘導する手段にもなっています。
診療報酬体系は、1927年の健康保険法施行に伴い公定価格として規定されたことに由来し、1958年には現行の診療報酬体系の基となる新医療費体系が導入されました。そして、高度経済成長期における医療技術の進歩や受診率の上昇により、医療費は1965年から1975年の10年間で約5.8倍に増加しました。このため1980年代以降、診療報酬改定率の抑制や入院医療費の包括払い(DPC/PDPS)化の推進などにより、医療費の抑制が図られました。
1990年代に入ると、高齢化の進行に対応するため医療制度改革が検討され、1997年に「介護保険法」が制定されました。2000年に介護保険制度が施行されると、診療報酬体系についても従来の入院料を統合した「入院基本料」が新設されるなど、包括化が推進されました。また、地域医療計画に基づく医療機関の機能分化や、重症度・看護必要度に応じた入院料の設定など、医療の質を評価する仕組みも導入されました。2006年には政府の「経済財政運営と改革の基本方針」に基づき、医療費適正化を目的として診療報酬の大幅なマイナス改定が行われました。 2012年には地域完結型の医療・介護サービス提供体制である地域包括ケアシステムの構築に向けた医療機関同士の連携強化が進められました。2020年には新型コロナウイルス感染症の拡大を受けてオンライン診療の評価が新設され、感染症対策への対応が図られました。
2024年の診療報酬改定では、「初診料」や「再診料」「入院基本料」が引き上げられ、こうした引き上げにより看護師、看護補助者、技師などのベースアップや40歳未満の勤務医、事務職員などの賃上げを行うとしています。また、急増している高齢者の救急搬送の受け皿として、リハビリや栄養管理を手厚くして早期の退院をサポートできる地域包括医療病棟が新設されます。日頃から介護保険施設と連携し、入所者の病状が悪化した際には、往診したり入院を受け入れる医療機関への加算が設けられました。一方、医療費抑制に向けて生活習慣病に関する報酬を再編し、生活習慣病管理料の請求を月1回のみとするほか、処方箋料の引き下げや受診しなくても医師の定めた一定の期間内であれば繰り返し使える「リフィル処方箋」の発行を促す加算の拡充も盛り込まれました。
今後の診療報酬改定の課題は、高齢化に伴う医療需要の増大への対応と、限られた医療資源の効率的活用です。団塊世代が75歳以上になり始める2025年頃からの医療体制の検討が求められます。医療機関の役割分担の明確化、医療の質を的確に評価する指標の充実、ICT技術の活用、医療従事者の育成・確保と勤務環境の改善なども重要な課題です。
メディアスグループは、医療機器の販売を中心とした事業を展開しています。医療に携わる私たち(Medical+us)は、医療現場や人々の健康的な明日へ役立つ情報をお届けする情報発信源(Media)の役割も果たしていきたいと考えています。