
Release date: 2022.10.18
October is Pink Ribbon Month, which calls for early breast cancer screening. Breast cancer is said to be common among people who are busy with child-rearing, nursing care, and work, but if it is detected early and treated early, a favorable prognosis can be expected. Therefore, we will summarize the examination of breast cancer in three parts. The first introduces types of cancer screening and mammography.
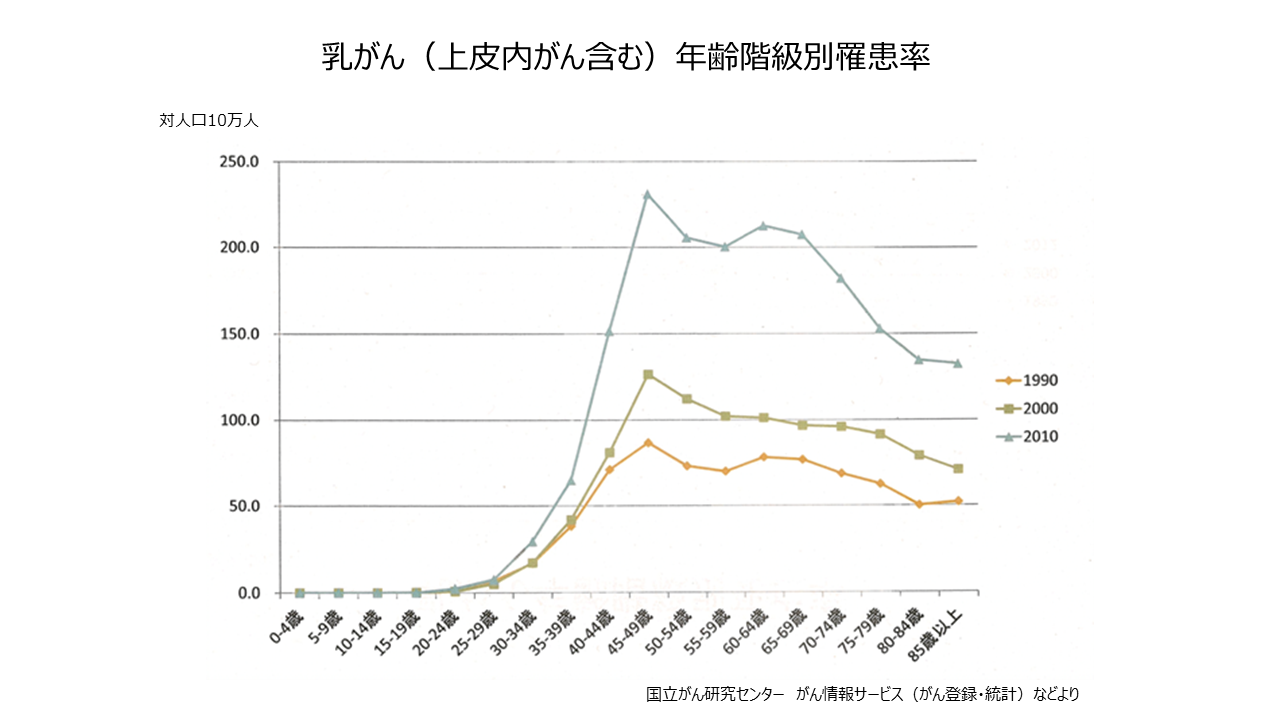
One in nine Japanese women will develop breast cancer. It increases from the late 30s, is common in the age group of 40 and over, and is the leading cause of cancer death among women in their 40s and 50s. Many of the affected people are said to be in a generation that is so busy with childcare, nursing care, and work that they put themselves off. Breast cancer continues to increase in incidence and mortality.
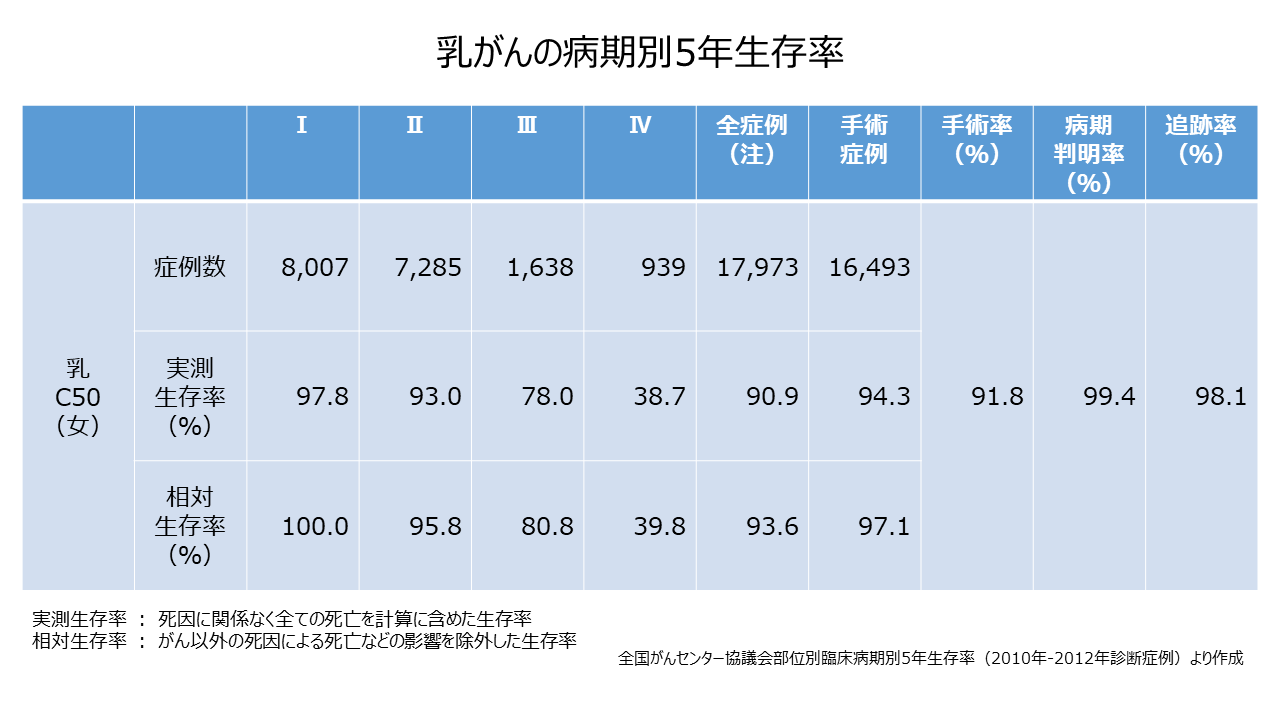
The five-year relative survival rate for early-stage breast cancer (Stage I) diagnosed in 2010-2012 is 100%, according to a National Cancer Center Council summary. If detected early, a good prognosis can be expected. Early detection of breast cancer is extremely important. One way to do that is by screening.
There are two types of cancer screening: the “countermeasure type” implemented by the national and local governments, and the “voluntary type” that individuals receive voluntarily. According to the government's policy, preventative breast cancer screening is targeted at people aged 40 and over, with a recommended screening interval of once every two years. Voluntary breast cancer screening is equivalent to comprehensive medical checkups. As a general rule, you pay for the examination yourself, and you can choose the examination according to your purpose and preference. According to the 2019 Comprehensive Survey of Living Conditions, the breast cancer screening rate was as low as 47.4%.
Breast cancer screening includes visual inspection, palpation, mammography (X-ray imaging), and ultrasound (echo). If there is a possibility of breast cancer, histopathological examination of the cells and tissues of the lesion under a microscope, CT (computed tomography) examination, MRI (magnetic nuclear magnetic resonance) to examine how the cancer spreads and metastasis resonance imaging), bone scintigraphy, and PET (Positron Emission Tomography).
During the inspection, the size and shape of the breast, twitching, swelling, and presence of abnormal discharge from the nipple are visually observed. During palpation, the doctor actually touches the breast to check for the presence, size, shape, hardness, and surface condition of a lump (tumor). In addition to the breast, check the lymph nodes under the armpit and above the collarbone.
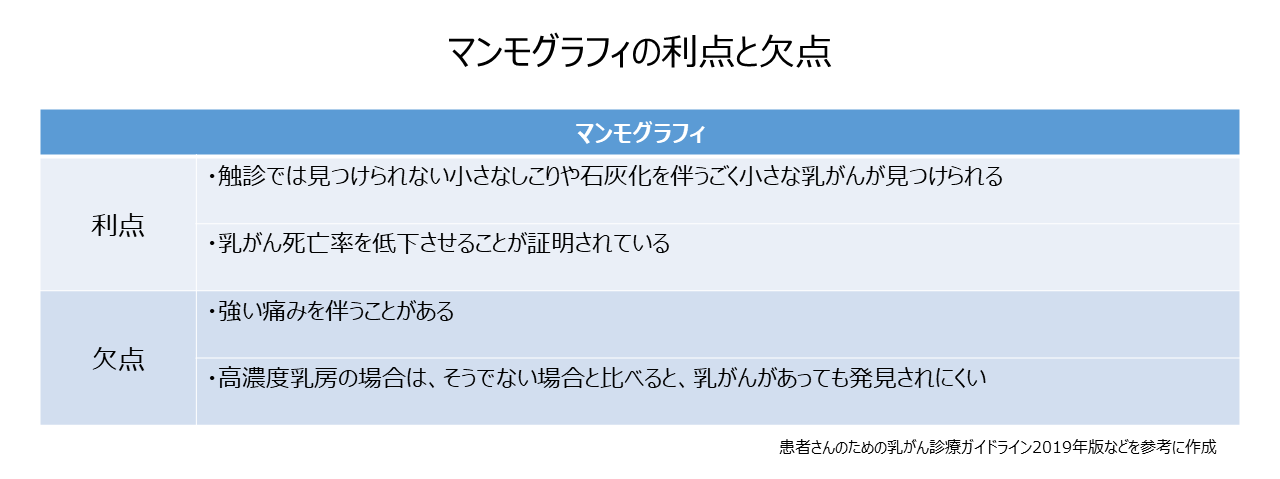
The standard screening method for breast cancer is mammography, which is considered to be effective in reducing mortality. A mammogram is an x-ray examination of the breast. For imaging, the breast is held with a plastic plate and an imaging table, stretched as flat as possible, and photographed from two directions, up, down, left, and right. Patients with breast tenderness may experience some pain during the examination. By stretching the breast thinly, the mammary glands spread and the slightly white lumps can be observed more clearly. Lumps may be benign or malignant, but if they cannot be distinguished by image diagnosis, they are determined by cytological examination. Mammography can detect very small breast cancers with small lumps or calcifications that cannot be detected by palpation.
In mammography images, the mammary glands appear white and the fat appears black, but lesions such as breast cancer also appear white. ), cancer tends to be difficult to detect because the lesion is hidden behind the white mammary gland. In your 40s, breast tissue begins to be replaced with adipose tissue. Therefore, it is said that ultrasonography is more suitable than mammography for people under the age of 30. The amount of radiation received by the breast from a single mammogram is about 1/50th of the natural radiation dose that the general public receives in a year, and is thought to have little effect on health. However, pregnant women should discuss with their doctor whether mammography is really necessary.

MEDIUS Group is developing a business centered on the sale of medical equipment. We (Medical + us) involved in medical care also want to play the role of an information source (Media) that delivers useful information for the medical field and people's healthy tomorrow.