ASOURCE®TIMES
救急車による救急搬送の件数は年々増え続けており、2019年には全国で約600万人が救急搬送された。高齢者の搬送が6割を占めており、それに伴い、応急処置について「本人や家族の意思を尊重するか否か」などの問題も増え、救急現場ではその対応に追われている。

今年の夏は、8月に入ってから全国的に気温が高い日が続き、熱中症の疑いで救急搬送される人が急増した。総務省消防庁によると、2020年6月1日から8月16日までに熱中症で救急搬送された人は、全国で3万5,317人。8月10〜16日までの1週間ではその約3分の1にあたる1万2,804人が救急搬送された。前週(8月3〜9日)の6,664人から倍増、前年同時期の7,639人をも大きく上回った。年齢別にみると、65歳以上の「高齢者」が61.8%を占め、次いで18歳以上65歳未満の「成人」が31.1%となっている。
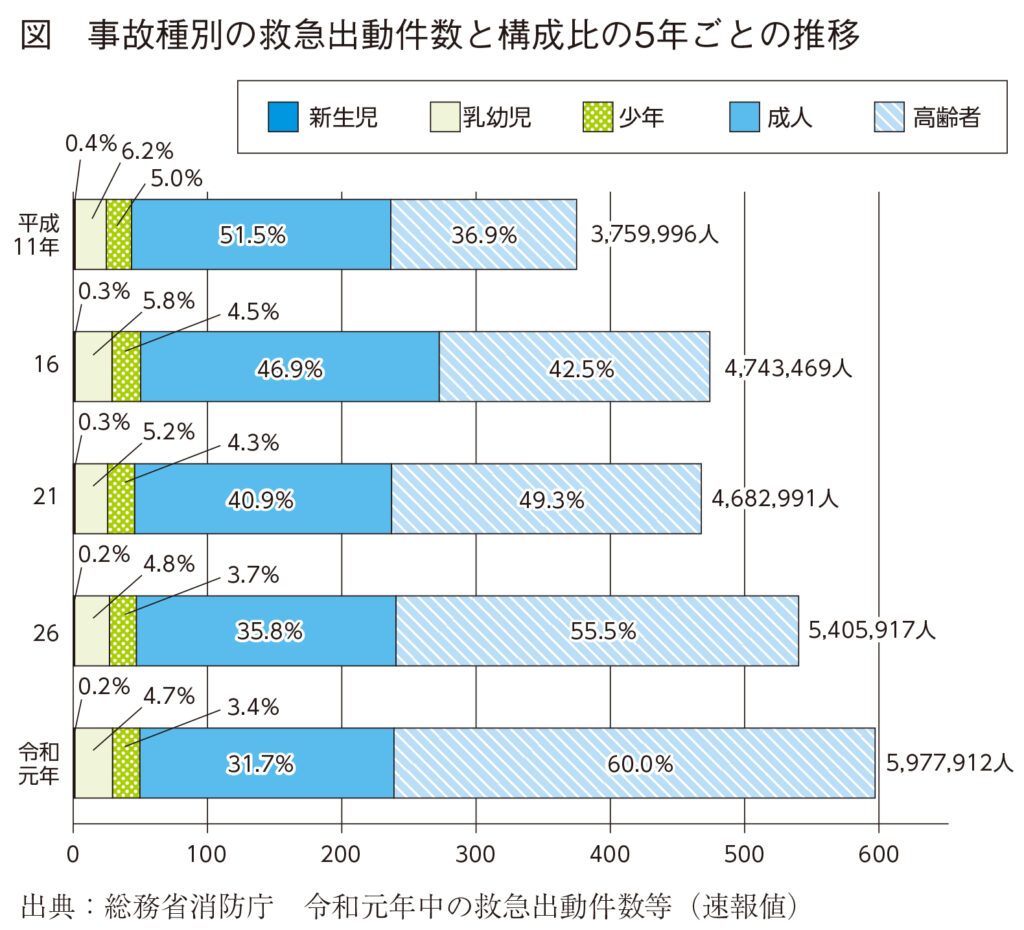
救急搬送では、近年、高齢者を搬送する件数が増え続けている。2019年の1年間に救急搬送された人は597万7,912人と過去最多を記録し、1999年からの20年間で約1.6倍に増加している(図)。高齢者の救急搬送も、人数、割合ともにこの20年間で1999年当時の2.6倍と増え続け、2019年は搬送者全体の60.0%が高齢者となっている。
こうした救急搬送の増加、高齢者の搬送者の増加は、人口の高齢化を反映した結果である。実際、救急車が出動する事故種別の割合を急病に限ってみると、1999年は全体の56.3%を構成していたが、2019年は65.3%と増加している。
急病が増加したのは、自宅や高齢者施設などで急に具合が悪くなり、救急車を呼ぶ高齢者が増えたためで、こうした搬送が増えるにしたがい、救急現場ではさまざまな問題が起きるようになった。
その一つが、心肺蘇生を望まない人への対応である。心肺停止の搬送件数も年々増え、そのうち60歳以上が85%、さらに80歳以上が半数を占めている。高齢者が多いので、救急現場では「本人は心肺蘇生を望んでいない」と家族から心肺蘇生の中止を要望されるケースが増えてきているのだ。一刻を争う状況の中で、救急隊が人命救助のために蘇生処置を行いながら救急搬送するか、本人の意思だという家族の意見を優先するか、判断に苦慮する事態が問題となっている。
平成25年度厚生労働科学研究の「救急業務における心肺蘇生の開始、中止に関わる現状に関するアンケート調査結果」によると、救急隊員の17%が、心肺停止状態の本人が、リビング・ウィルなどの書面によって心肺蘇生を希望しない意思を示している事例を経験していた。一方で、心肺蘇生の不実施(DNAR=Do Not Attempt Resuscitation)を表明している人への救急隊の対応は各消防本部によって異なり、総務省消防庁が2018年に実施した調査では、DNARへの対応方針を定めていない消防本部が54.4%に上った。
こうしたことから、本人の終末期の希望や意思を可能な限り尊重するために、厚生労働省、日本臨床倫理学会、日本集中治療学会などの学会、関連団体が、DNARを含む終末期医療に関するガイドラインを提言している。しかし、これらのガイドラインの対象は、急変時に救命医療を施せる、あるいは医師によるDNAR指示ができる医療機関の入院患者に限られている。急病で救急車を呼ぶ高齢者の大半が自宅あるいは高齢者施設にいるため、救命医療が直ちに行えず、本人のDNARの意思の確認や、医師によるDNAR指示を救急隊員がどう取り扱うべきか、いまだ定まったガイドラインはない。
このような状況の中、東京消防庁では2019年12月から、かかりつけ医らの指示によるDNARを導入する方針を示した。家族や医師らで「人生会議(ACP)」を行った成年で、心肺停止状態にあること、本人が悪性腫瘍の末期など人生の最終段階にあること、本人に「心肺蘇生の実施を望まない意思」があることなどの条件が必要となる。この方針により、家族が患者の急変(心肺停止)に慌てて救急車を呼んでしまっても、救急隊はまずかかりつけ医に連絡し、かかりつけ医が死亡を確認するという流れができるため、本人の意思が尊重されるケースが増えると期待されている。
高齢者の救急搬送でもう一つ問題となるのが、救急車の「不適正な利用」である。例えば、東京消防庁によると、実際にあった高齢者の救急車の出動要請の理由として「病院に入院する予定になっているが、自分で行くとタクシー代がかかるので救急車を呼んだ」や「眠れなくて、誰かに話を聞いてほしくて救急車を呼んだ」などがあった。
不適正な救急車の利用があると、必要な救急車の台数が不足し、救急搬送に要する時間が増加することになる。実際、救急車の現場到着平均所要時間は、2009年が7.7分であったのに対し、2019年では8.7分と1分延伸し、救急隊が到着してから病院へ収容するまでの平均時間も、2009年は35分であったのに対し、2019年は39.5分と4.5分も増加している。最近ではCOVID-19の対応に加えて、こうした救急車の不適正な利用の増加に伴い、病床やスタッフが足りずに救急患者が受入困難になる問題も増加している。
総務省消防庁によると2009〜2019年の10年間で、救急搬送されたが軽症と診断された患者は、救急搬送全体の50%ほどで比率にあまり増減がない。しかし、軽症と診断された高齢者の患者は34.1%から49.0%と、15ポイントの増加があった。かつては、救急車で搬送された患者のうち、外来診療だけで帰宅できた患者=軽症者=不適正な利用者と考えられていたが、軽症者が増えたのは不適正な利用だけが理由ではなく、従来なら入院していた傷病でも、診断・治療の技術の進歩によって、外来で十分対応でき、帰宅できるようになった人が増加してきたためとも考えられる。
ただ、「歩ける状態になったからといって、患者をすぐに帰宅させるかどうかは、慎重に検討・対応する必要がある」と指摘するのは、国際医療福祉大学医学部教授(同大学病院救急医療部)の志賀隆氏だ。実際にあった症例として、救急搬送された70代の女性を挙げた。主訴は脱力感。頭痛、胸痛、発熱はなく、軽度の低ナトリウム血症と脱水が認められたため、点滴を開始したところ「もう元気になったから、点滴を抜いて帰りたい」と言い出したという。独居、自宅まで5km、財布には500円などの状況から、まず地域包括支援センターに連絡したところ、よく知っている住民との返事があり、その後の対応を任せたという。「帰宅できても、日常生活は誰かのサポートが必要な高齢者は少なくない。救急現場では、そうした状況も考慮した対応が求められる」と志賀氏は言う。限られたリソースの中での細かな対応力も、救急医療で求められることの1つであるのだ。
事故種別の救急出動件数と構成比の5年ごとの推移
出典:総務省消防庁 令和元年中の救急出動件数等(速報値)
救急車は、患者を安全に運び、救急隊員が動きやすいようにと、時代を追ってさまざまな点が改良されてきた。1970年代には交通事故が増え、患者を病院に運ぶまでの止血や酸素吸入などの応急処置に対応するために、救急車にはいろいろな機器が備えつけられるようになった。
現在では「高規格救急車」が標準になりつつある。高規格救急車は1992年に救急救命士制度が導入される前後から開発が進んだ。車内は動きやすいように天井の高い車が導入され、車の揺れも少なくなり、寝台(ストレッチャー)も備えつけられた。車内には救命行為に必要なさまざまな機器が設置されている。処置に必要な気道管理用セットや分娩セット、PPEなどの医療機器のほか、患者監視装置(心電図・脈波・血圧・血中酸素飽和度)、自動式体外除細動器、人工呼吸器なども搭載している。これらの設備・機器の進歩により、医師の指示や助言のもとに、現場や車内で行える救命処置が拡大し、患者の救命率向上が期待されている。

 救急車内の医療機器
救急車内の医療機器